Latent Tuberculosis Infection (LTBI)
Purpose of this blog:
To make general public and general/family physicians aware about this entity so as to avoid unnecessary testing for LTBI and treatment with anti-TB drugs.
What is Latent Tuberculosis Infection?
Latent tuberculosis infection (LTBI) is defined as a state of persistent immune response to stimulation by Mycobacterium tuberculosis antigens with no evidence of clinically manifest active TB.
In simple terms,
Latent tuberculosis infection (LTBI) is the presence of Mycobacterium tuberculosis in the body without signs and symptoms, or radiographic or bacteriologic evidence of tuberculosis (TB) disease.
Is there a test for latent TB infection?
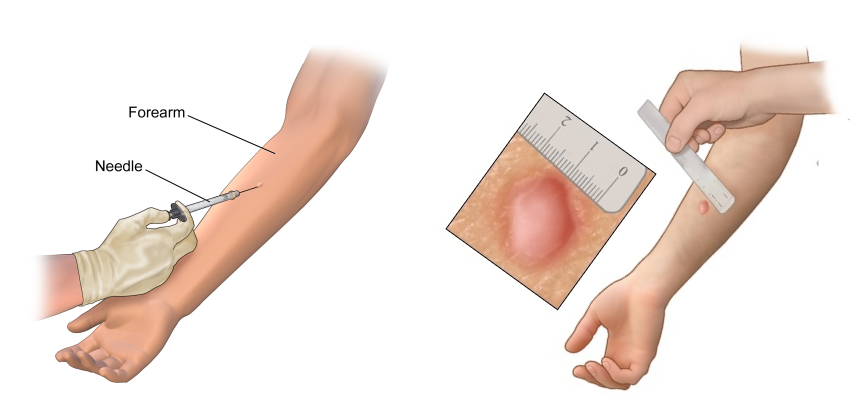
Tuberculin skin test (Mantoux test) and Interferon gamma release assay (IGRA – TB gold/ Gold QuantiFERON)
However, one must know there is no gold standard test for LTBI.
Also, TST / IGRA are not used as diagnostic test for active tuberculosis disease.
What is recommendation for testing and treating people LTBI? World health organization and Indian recommendations.
India, with one-fourth of the global burden of TB, has 40 per cent of the population infected with M.TB.
Treating 40 per cent of the population for LTBI based on Tuberculin
Skin Test (TST) positivity or Interferon Gamma Release Assay is neither rational nor practicable, hence focused approach is needed.
World health organization recommends screening in following population.
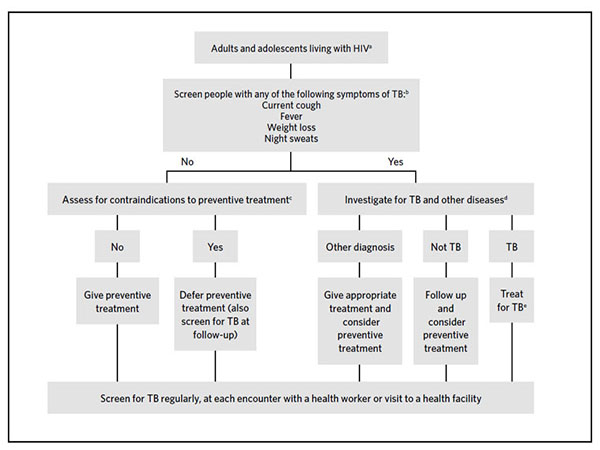
- 1. Adults, adolescents, children and infants living with HIV
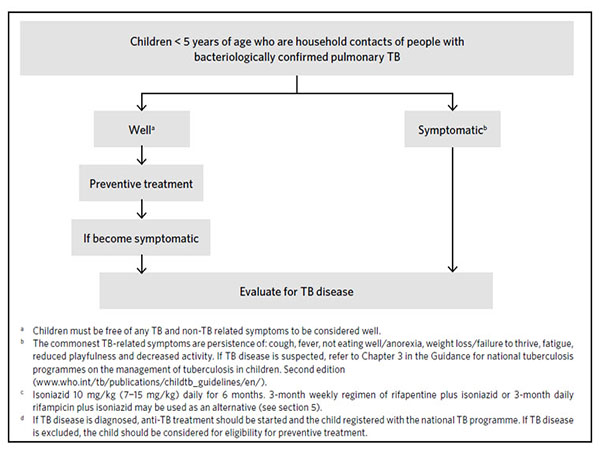
- 2. HIV-negative children aged < 5 years (<6 years in INDIA) who are household contacts of people with bacteriologically confirmed pulmonary TB.
- 3. Other HIV-negative at-risk groups (As per World health organization, not included in Indian guidelines yet)
- a. Patients initiating anti-TNF treatment, patients receiving dialysis, patients preparing for an organ or hematological transplant and patients with silicosis should be systematically tested and treated for LTBI. (Receiving long term corticosteroids – Included in NTEP).
- b. In countries with a low TB incidence, systematic testing for and treatment of LTBI may be considered for prisoners, health workers, immigrants from countries with a high TB burden, homeless people and people who use illicit drugs
- c. Systematic testing for LTBI is not recommended for people with diabetes, people with harmful alcohol use, tobacco smokers and underweight people unless they are already included in the above recommendations.
In India, as per National Tuberculosis Elimination Programme
People living with HIV and children less than 6 years, need not be checked by TST or IGRA for latent TB. Treatment can be initiated after excluding active TB disease. Isoniazid treatment for 6 months is required.
Studies have demonstrated that Isoniazid (INH) taken for at least 6 months in persons with LTBI reduced subsequent TB incidence by 25 to 92 per
cent, the differences in effectiveness largely explained by differences in treatment completion.
In clinical situations, the most obvious group for LTBI treatment would include high-risk patients such as those receiving long term corticosteroids, immunosuppressants, HIV-infected and juvenile contacts of sputum-positive index cases.
Differentiating Between and Latent TB infection and TB disease.
| Latent TB Infection | <TB Disease |
|---|---|
| No symptoms or physical findings suggestive of TB disease. | Symptoms may include one or more of the following: fever, cough, chest pain, weight loss, night sweats, hemoptysis, fatigue, and decreased appetite. |
| TST or IGRA result usually positive. | TST or IGRA result usually positive |
| Chest radiograph is typically normal | Chest radiograph is usually abnormal. However, may be normal in persons with advanced immunosuppression or extrapulmonary disease. |
| If done, respiratory specimens are smear and culture negative. | Respiratory specimens are usually smear or culture positive. However, may be negative in persons with extrapulmonary disease or minimal or early pulmonary disease. |
| Cannot spread TB bacteria to others. | May spread TB bacteria to others. |
| Should consider treatment for LTBI to prevent TB disease. | Needs treatment for TB disease. |






